Mitochondrial involvement.
The purpose of this review is to describe the current understanding of variations in mtDNA or nuclear DNA that impact on mitochondrial-related gene expression reported in schizophrenia (SZ), bipolar disorder (BPD), and major depressive disorder (MDD).
Recent findings of mitochondrial abnormalities in brains from subjects with neurological disorders have led to a renewed search for mitochondrial abnormalities in psychiatric disorders. A growing body of evidence suggests that there is mitochondrial dysfunction in schizophrenia, bipolar disorder, and major depressive disorder, including evidence from electron microscopy, imaging, gene expression, genotyping, and sequencing studies. Specific evidence of dysfunction such as increased common deletion and decreased gene expression in mitochondria in psychiatric illnesses suggests that direct examination of mitochondrial DNA from postmortem brain cells may provide further details of mitochondrial alterations in psychiatric disorders.
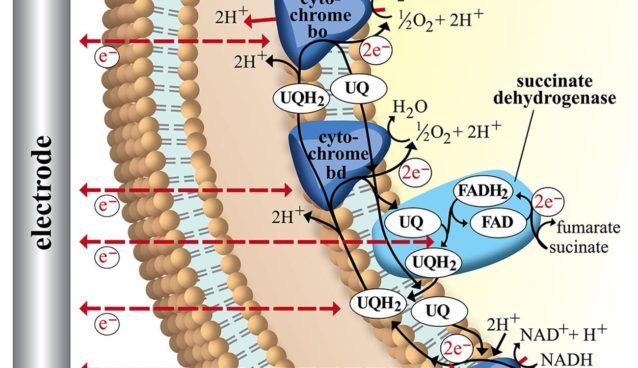
The mitochondrion is a subcellular organelle located in the cytoplasm of all cells and contains copies of mitochondrial DNA (mtDNA). MtDNA encodes two ribosomal RNAs, 22 transfer RNAs, and 13 protein subunits of the electron transport chain and the displacement loop (D-loop), which is necessary for replication and transcription of the mitochondrial genome. In addition to the small number of genes encoded within the mitochondrion, it is estimated that at least 1000 nuclear-encoded proteins are also translocated to the mitochondria. The interactions between both mitochondrial proteins and translocated proteins are required for normal cellular function. MtDNA is 16,569 base pair circular DNA with a guanine-rich heavy (H) strand and a cytosine-rich light (L) strand. The remaining subunits of the electron transport chain are encoded in the nuclear genome, which is physically separate from the cytoplasmically located mitochondrial genome. Each cell contains multiple mitochondria, and there are multiple copies of mtDNA in each mitochondrion. Muscle, brain, and liver often contain the highest number of mitochondria due to high energy utilization. Mitochondria provide energy for cellular processes by converting metabolites to adenosine triphosphate (ATP) via oxidative phosphorylation (OXPHOS). Mitochondria contain a highly permeable outer mitochondrial and a virtually impermeable inner membrane. The electron transport chain produces a pH gradient across the inner mitochondrial membrane that is important for ATP production and metabolite transport. OXPHOS is carried out by the five protein-lipid enzyme complexes of the respiratory chain, which are located in the inner membrane: complexes I (NADH: ubiquinone oxidoreductase), II (succinate: ubiquinone oxidoreductase), III (ubiquinol: ferrocytochrome c oxidoreductase), IV (ferrocytochrome c: oxygen oxidoreductase or cytochrome c oxidase), and V (ATP synthase).
Although mtDNA mutations may be maternally transmitted, they are often sporadic. MtDNA is more susceptible to somatic deletions than nuclear DNA because mtDNA is not protected by histones and also has a poor DNA repair system. Thus mtDNA has been suggested as a potential ‘weak point’ of the genome. Examples of clinical syndromes related to mtDNA mutations include Leber hereditary optic neuropathy (LHON), which is associated with a number of ND1 (see list of abbreviations) gene mutations, and myopathy and diabetes mellitus which are associated with point mutations in mitochondrial tRNA.
Although any organ can be affected by mitochondrial defects, the brain, skeletal muscle, and cardiac muscle are most commonly affected due to their high aerobic activity and higher mitochondrial content.The evidence for involvement of mitochondria in neurodegenerative disorders such as Alzheimer’s, Parkinson’s, multiple sclerosis, and amyotrophic lateral sclerosis has been recently reviewed and is not the focus of this review.
Evidence for mitochondrial dysfunction in psychiatric disorders.
Psychiatric symptoms of mitochondrial disease.
Psychiatric symptoms have been documented in subjects with mitochondrial disease. In a review by Fattal et al. 2006, the authors identified 19 confirmed case reports of mitochondrial disease with comorbid psychiatric problems, including MDD, psychosis, BPD, anxiety disorders, and personality change. Depression is a common symptom of the mitochondrial disease CPEO. A high comorbidity of mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes (MELAS) in SZ and bipolar affective disorder has also been documented.
Ultrastructure studies of mitochondrial abnormalities in psychiatric illness.
Electron microscopy studies have revealed mitochondrial abnormalities in SZ. Uranova et al. (2001) studied mitochondrial volume density in oligodendrocytes in the prefrontal cortex and caudate nucleus in postmortem brains of subjects with SZ and observed a significant decrease in mitochondria number and density in both regions in subjects with SZ compared to controls.
They observed a lower number of mitochondria in patients who were not taking antipsychotic medications compared to those taking antipsychotics or controls, suggesting drug treatment normalized mitochondria number.
Subjects with SZ were also observed to have monocyte and lymphocyte mitochondria that appeared swollen compared to those of controls. The same authors observed a significant increase in mitochondria density in lymphocytes and monocytes of neuroleptic-treated subjects with SZ compared to controls.
Research suggests antipsychotic treatment may be related to increased antiapoptotic effects mediated by mitochondrial signals. Expression of antiapoptosis genes Bcl-2 and Bcl-xL is increased by haloperidol treatment, and both prevent the release of proapoptotic substances such as cytochrome c. It is possible that these antiapoptotic effects may be compensatory to the effects of antipsychotics on mitochondrial respiratory chain complex expression.
Altered metabolic activity.
Decreased intracellular pH and intracellular phosphocreatine in the frontal lobes as well as an altered response of phosphocreatine response to photic stimulation have been observed in patients with BPD. Also, mRNA of two isoforms of creatine kinase, the enzyme that is involved in synthesis and metabolism of phosphocreatine, has been shown to be downregulated in the dorsolateral prefrontal cortex in subjects with BPD, although significant downregulation of these isoforms was not seen between subjects with SZ and controls.
Positron emission tomography (PET) scans with [18F]-fluoro-deoxy-glucose (FDG) have revealed altered metabolic decreases in SZ, BPD, and MDD. Hypofrontality, increased left and decreased right lentiform nucleus metabolic rate, and decreased temporal lobe metabolic rate have been reported in subjects with SZ compared to controls. In major depressive disorder, reduced metabolic rate has been observed in the prefrontal cortex, anterior cingulate cortex, and caudate nucleus in depressed patients.
Similarly, depressed subjects with BPD display reduced whole-brain metabolism compared to manic subjects with BPD. Depressed subjects with BPD have also been shown to exhibit decreased total frontal lobe metabolism and medial temporal lobe metabolism. Increases in metabolism in the frontal lobe and medial temporal lobe have been reported during mania in BPD. Thalamus and occipital lobe metabolism has also been shown to be altered in subjects with BPD, although again these findings are also state-specific.
Altered mitochondrial gene expression in psychiatric disorders.
A broad mitochondrial dysfunction has been reported in neuropsychiatric disorders using microarray technology to survey nuclear-encoded gene expression. One study of BPD found mitochondrial gene expression was predominantly decreased in BPD compared to controls in the dorsolateral prefrontal cortex (DLPFC) when using Stanley samples with pH above 6.5. In a select subgroup of medication-free BPD patients there were mitochondrial genes that showed increased expression. The authors suggested that medication may influence the direction of gene expression change and the precise genes altered in BPD patients; however, this subgroup of medication-free patients showed an increased brain pH as compared to controls. Since the contrast was not balanced between groups for pH, the interpretation that medications were driving the gene expression in the opposite direction can be explained equally by the strong effect of pH.
Two independent groups of researchers demonstrated in controls there were mitochondrial gene expression differences based upon mean group pH differences. Mexal et al. (2006) showed that hippocampal gene expression was highly dependent upon pH, especially for functional groups related to mitochondrial energy metabolism.
The findings of alterations in mitochondrial transcript expression appeared to be independent of the common deletion as there were no significant correlations between mitochondrial gene expressions for the 13 transcripts with the levels of common deletion. However, the direction in the data suggests that an increased common deletion is associated with decreased mitochondrial gene expression.