Lithium, Inositol and Mitochondria.
The inositol depletion hypothesis, introduced by Berridge et al., suggested that the mood-stabilizing effect of the drug is mediated by its inhibitory effect on several enzymes in the phosphatidylinositol (PI) cycle, mainly an uncompetitive inhibition of inositol monophosphatase (IMPase). Berridge et al. proposed that inhibition of IMPase would, consequently, lead to down-regulation of the PI cycle and dampening of the cleavage of phosphatidylinositol 4,5-bisphosphate (PIP2) upon activation of several G-protein coupled receptors into the two second messengers, inositol trisphosphate (IP3) and diacylglycerol (DAG). Thus, lithium treatment would result in regulation of cellular signaling induced by assumingly hyperactivated neuronal receptors in the brain.
However, extensive studies of the effects of lithium mediated by inositol depletion suggest that these effects expand beyond regulation of cellular signaling per se. Sarkar and co-workers demonstrated that inositol-depletion results in induction of autophagy, a cellular mechanism responsible mainly for the clearance of aggregated and misfolded proteins as well as dysfunctional organelles.
We have recently addressed the issue of downstream effects of lithium mediated by intervention in inositol metabolism by comparing changes in gene expression induced by lithium treatment with those induced by knockout of either of two genes encoding for proteins involved in the PI cycle. The main finding of the study was that the only common effect observed in all three groups (lithium-treated mice and the knockouts of each of the two genes) is up-regulation of genes related to mitochondrial function.
We were also able to demonstrate that mild chronic inhibition of mitochondrial function with low rotenone doses that do not affect general behavior or well-being of the animals enhanced amphetamine-induced hyperactivity and interfered with the antidepressant effect of lithium in the forced swim test model of behavioral despair. Moreover, the hyperactive response to amphetamine in rotenone-treated animals could be completely abolished by chronic lithium treatment.
While our study supports previous reports regarding hampered mitochondrial function in bipolar patients and beneficial effects of lithium on mitochondrial function, it also raises two speculations.
Previous observations of aberrant mitochondrial function in bipolar patients leave a causality relationship between mitochondrial dysfunction and bipolar disorder an open question. On the other hand, our behavioral results following rotenone treatment tempt us to speculate that mitochondrial dysfunction predisposes manic behavior and that drugs targeted to ameliorate mitochondrial function are potential preventers of bursting manic episodes. Our results also suggest that damaged mitochondrial function per se is not sufficient to alter behavior; rather, it sensitizes the response to certain triggers. It may not be ruled out that prolonged mitochondrial dysfunction would, eventually, affect other cellular processes and/or alter the function of proteins or even induce cell death, all of which are potential triggers of abnormal behavior.
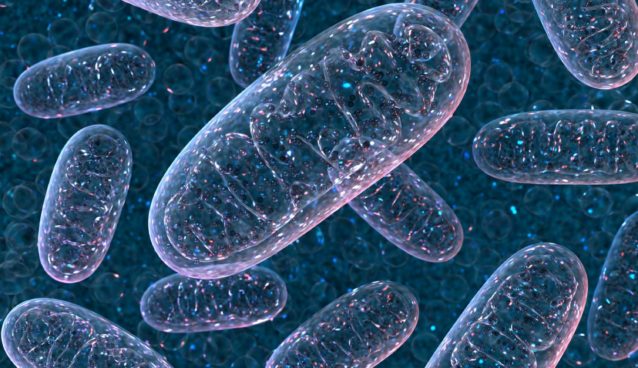
The mechanism mediating the positive effect of modified inositol metabolism on mitochondrial function is unclear. One possibility is that the beneficial effects are obtained by enhancement of autophagy, induced by inositol depletion. Mitochondria undergo cycles of fission (segregation into two daughter organelles) and fusion (assembly of two organelles into one). Fission events frequently result in unequal segregation into more and less functional daughter mitochondria and sequestration of the dysfunctional organelles via selective degradation by autophagy (mitophagy). It is conceivable that the inositol depletion-mediated enhanced autophagy would result in enhanced clearance of damaged mitochondria and accelerated new mitochondria biogenesis from “healthy” organelles, thus increasing the proportion of fully functional organelles. Increased mitochondrial turnover stands align with the general up-regulation of mitochondrial genes observed in lithium treated mice and in PI cycle-related knockout mice, as well as with upregulation of mitochondrial integrity protein markers observed in these mice.
Mitochondrial dysfunction has also been implicated in neurodegenerative disorders including Parkinson’s disease, Alzheimer’s disease, Huntington’s disease, and amyotrophic lateral sclerosis (ALS). Interestingly, the pathophysiology of all of the above disorders also involves impaired autophagy. In addition, numerous studies report altered mitochondrial function in schizophrenia and major depressive disorder.
On the other hand, if mitochondrial dysfunction and aberrant autophagy are indeed involved in all the disorders mentioned above, what makes them to present distinct phenotypes?