Inflammation and Bipolar.
Over the past decade, bipolar disorder has been consistently associated with clinical comorbidities . Recent data from the Systematic Treatment Enhancement Program for Bipolar Disorder show that over 50% of patients with chronic bipolar disorder have at least one associated comorbidity. Prominent in this group are cardiovascular disease, diabetes, obesity, dyslipidemia, and insulin resistance – all metabolic syndrome components . This overlap is one of the reasons why great emphasis has been placed on systemic mechanisms related to bipolar disorder-related impairment . Up to the present moment, two clinical studies, one conducted at a specialized clinic and another assessing the general population , have shown that subtle proinflammatory states are characteristic of the peripheral pathophysiology of bipolar disorder .
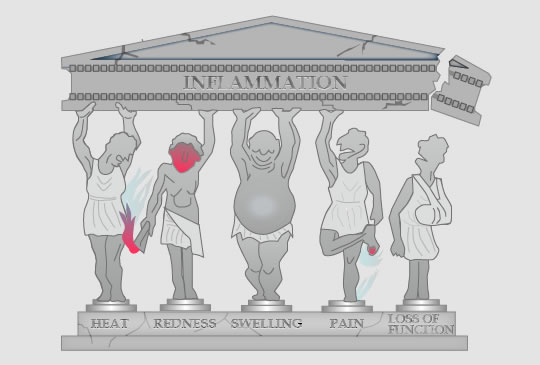
The immune system is often involved with inflammatory disorders, such as allergic reactions and skin disorders, many of which result in abnormal inflammation. Wounds and infections would never heal without inflammation, but chronic inflammation, if not controlled, can also lead to a number of pathological conditions, such as inflammatory bowel disease and rheumatoid arthritis. This is one of the reasons why the inflammation is so closely regulated by the body.
Inflammation is a part of the nonspecific immune response that takes place after any type of bodily injury or microbial invasion. Many of these reactions involve cytokines, especially interleukin-1 (IL-1), tumor necrosis factor-alpha (TNF-α) and IL-6, produced by dendritic cells, macrophages, and other types of cells. Inflammatory responses are also accompanied by increased levels of acute-phase reactants [such as high sensitivity C-reactive protein (hsCRP)] and complement factors .
Progressive impairment of different cognitive functions has been consistently described in bipolar disorder, corroborating a potential role of neuroinflammation in this illness. Immune signaling in the brain is of special interest because it provides a relevant explanatory link between progressive dysfunction, cognitive impairment, medical comorbidity, and premature mortality. Neurocognitive alterations include impairment of attention, executive function, and verbal memory. These changes can be influenced by inflammatory mediators through the shaping of synaptic transmissions. Inflammation can influence the role of microglia in synaptogenesis (synaptic formation) and pruning, that is, reduction of the overall number of neurons and synapses, leaving only more efficient synaptic configurations. Also, TNF-α influences dendritic arborization, modulates long-term potentiation (a mechanism of memory consolidation), and affects neurotransmitter pathways.
Because the pathophysiology of bipolar disorder tends to differ in early versus late stages, the term neuroprogression has been used to describe these changes. Structural and functional modifications change as the illness progresses and as patient age increases. MRI studies have suggested abnormal neural development already in the early stages of the disorder, with progressive changes as mood episodes occur. Neuroprogression in bipolar disorder underlies changes in inflammatory cytokines and neurotrophins, mitochondrial dysfunction, oxidative stress, and epigenetic effects. These parameters can be sensitive to the progression of illness and have, therefore, been used as first biochemical indicators in the staging of bipolar disorder.
The brain is rich in resident macrophages, called microglia, which become activated in response to tissue damage or brain infections and can be the first to detect critical changes in neuronal activity and health.The threshold for microglial activation, however, may be higher than that of macrophage activation in other tissues. Healthy neurons maintain microglia in an inactive state via secreted and membrane-bound signals, including CD200, CX3CL1 (fractalkine), neurotransmitters, and neurotrophins. If this control fails (e.g., as a result of neuronal injury or loss of regulatory signals), activated microglia may participate in a form of chronic neuroinflammation, which has been implicated in the pathoetiology of a number of neurodegenerative diseases.
A 2010 study reported that markers of neuroinflammation were significantly upregulated in post-mortem frontal cortex from patients with bipolar disorder. In particular, those authors observed the activation of the IL-1 receptor (IL-1R) cascade involved in microglial activation. The same work found increased astroglial and microglial markers (glial fibrillary acidic protein, inducible nitric oxide synthase, c-fos, and CD11b), another evidence of microglial activation [22]. Recently, patients experiencing one or more manic/hypomanic episodes during the previous year were shown to have significantly higher levels of IL-1β in cerebrospinal fluid levels when compared with patients without a recent manic/hypomanic episode. This indicates a relationship between the presence of acute episodes and activation of the IL-1R cascade.
There is considerable preliminary evidence suggesting that traditional mood stabilizers modulate neuroinflammation. Very recently, lithium was shown to have neuroprotective activity in two preclinical studies.
The adjunctive use of drugs with anti-inflammatory properties, such as omega-3 fatty acids (fish oil), COX inhibitors, minocycline, and statins, is another arena that has recently started to be explored. Omega-3 are nutritionally important fatty acids that include α-linolenic acid (C18 : 3), docosahexaenoic acid (DHA, C22 : 6), and eicosapentaenoic acid (EPA, C20 : 5). A recent meta-analysis showed that EPA is a more effective component in the treatment of major depressive episodes than DHA. These molecules are supposed to compete for the biotransformation of inflammatory eicosanoids (such as prostaglandins and leukotrienes). In fact, competition for the biosynthesis of inflammatory mediators could be partially responsible for their anti-inflammatory effects. Although current evidence does not support the adjunctive use of omega-3 in the treatment of bipolar mania, some studies have demonstrated its efficacy in bipolar depression.
Acetylsalicylic acid (ASA) irreversibly inhibits COX-1 and modifies the enzymatic activity of COX-2. COX-1 and COX-2 differentially modulate leukocyte recruitment during neuroinflammation. The clinical use of low-dose ASA has been primarily driven by its role as an antithrombotic and thrombolytic agent. Given the high rates of death from cardiovascular events in bipolar disorder, this action might be potentially advantageous in the management of bipolar disorder.