Cannabis-Induced Bipolar Disorder with Psychotic Features
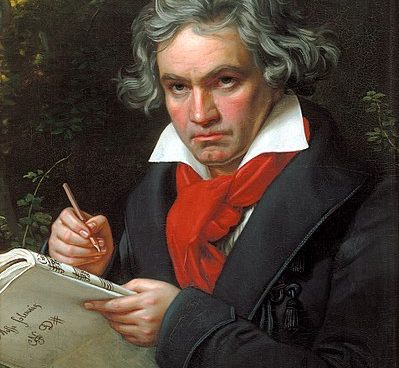
“Never misjudge the most faithful heart of your beloved.” – Ludwig van Beethoven.
Case study.
Peter was a 21-year-old, who presented to our facility for his second psychiatric hospitalization. He was discharged one week prior after a 30-day stay with a diagnosis of cannabis-induced psychotic disorder. He started using cannabis shortly afterward and became symptomatic with more pronounced delusions and psychotic behavior.
He had pressured speech, racing thoughts, flight of ideas, insomnia, and delusions of grandeur that he “owns this hospital” and worked as a “successful rap artist.” His physical exam was unremarkable except for his urine toxicology, which tested positive for cannabis.
During his first psychotic break, his girlfriend notified the police that he had been hearing voices lately and was fearful that he may be a threat to others. She reported that he was acting increasingly delusional and suspicious since his trip from Cuba—making statements that people were out to get him and had planted a microphone in his stomach to broadcast his thoughts.
He was diagnosed with cannabis-induced psychotic disorder since his symptoms occurred during the time he was smoking cannabis. Also, his initial psychotic behavior quickly subsided upon his arrival to the hospital.
He reported hearing voices from these microphones that were running a commentary on his life telling him repeatedly “you’re over.” These auditory hallucinations, which he referred to as “reverb,” had only occurred when he smoked cannabis.
Substance use/abuse history. Peter started using cannabis when he was 16-years old. He only used it rarely in the past, but started using it on a daily basis in the past few months and in greater quantities. He began using alcohol when he was 14-years old. He typically drank (“a few beers”) on the weekends. He did not report passing out or withdrawal seizures. He denied any other illicit drug use.
Family history. There was no reported psychiatric illness in his family.
This time he displayed delusional ideations, extreme grandiosity, and mood lability. He was hospitalized for a duration of four months. During the first two months, he refused to take any medications and continued to display this same bizarre behavior. In addition, he appeared to be internally preoccupied and would stare at himself and talk to himself for hours at a time. His diagnosis was soon changed to bipolar disorder with psychotic features.
He was administered and responded quickly to olanzapine orally disintegrating tablets and valproic acid liquid which was later changed to olanzapine 15mg orally, twice daily and divalproex sodium 750mg orally, at bedtime.
Upon discharge, Mr. X was asymptomatic with no residual signs of psychotic or affective symptoms.
Q.What is the link between cannabis and the endocannabinoid system.?
Cannabis has a major psychoactive component, Δ9-tetrahydrocannabinol (Δ9-THC).
During the last 20 years, endogenous receptors for Δ9-THC, cannabinoid receptors (CB1 receptors in particular for neuronal functions) and endogenous ligands (called endocannabinoids) have been discovered.
It has now been recognized that the endocannabinoid system (comprising cannabinoid receptors, endocannabinoids and a synthesizing and degradation machinery for endocannabinoids) represents a novel signalling system in the nervous system, regulating numerous processes, from neural development to synaptic transmission processes.
At present, the notion is put forward that endocannabinoids are locally produced and are able to regulate neural progenitor proliferation and specification of pyramidal neurons via activation of CB1 receptors. This receptor is also involved in controlling axonal navigation, neuronal migration and positioning of GABAergic interneurons and excitatory neurons. These insights were gained from studies in rodents, where components of the endocannabinoid system were genetically inactivated, or by pharmacological treatments with CB1 receptor antagonists. Besides the exciting insight that endocannabinoids and their receptors are involved in numerous central steps in neural development.
Q.What are the mechanisms underlying the devastating effects of cannabis consumption during critical phases of brain development.?
As endocannabinoid levels are tightly regulated in time and space to execute their ascribed roles, Δ9-THC consumption leads to a strong disturbance of the endocannabinoid system. Δ9-THC activates all CB1 receptors in the body irrespective of there current intrinsic activation pattern. Secondly, while endocannabinoids undergo a fast degradation, Δ9-THC is rather stable and occupies CB1 receptors for a long time.
Q.What are the effects cannabis can have during the phase of brain development.?
The period of the brain growth spurt (in rats: from birth to postnatal day 21; in humans: third trimester of pregnancy to first 2 years of life) is particularly sensitive to Δ9-THC. Even a single injection of a synthetic CB1 receptor agonist at the peak of the brain growth spurt (i.e. on postnatal day 10 in rats) can lead to long-lasting behavioural changes, including anxiety-related and depressive-like behaviour.
Q.What are the neurobiological consequences of maternal marijuana use on foetal development in humans.?
CB1 receptors are highly expressed in mesocoticolimbic areas in the midgestation human foetal brain. These neuronal systems are relevant for mood, cognition, reward and goal-directed behaviours. A majority of studies, in fact, have observed that newborns and infants born to cannabis users have increased tremors, exaggerated startle responses and poor habituation to novel stimuli. By the age of 10, prenatal marijuana-exposed children were reported to have increased hyperactivity, inattention and impulsive symptoms. Regarding psychiatric disorders, emerging evidence is present that maternal cannabis exposure also predicts early onset and increased frequency of cannabis use. To detail molecular mechanisms underlying this effect, human foetal brain after cannabis exposure showed discrete neuronal disturbances on, e.g. striatopallidal circuits (i.e. decreased expression of proenkephalin and dopamine D2 receptor).
Q.What is the association between cannabis use and psychosis.?
Clear evidence is provided that acute cannabis treatment can induce transient schizophrenia-like positive, negative and cognitive symptoms in some healthy individuals. The mechanisms underlying these effects may involve dopamine, GABA and glutamate transmission. Regarding the emergence of schizophrenia after frequent cannabis use, only a small proportion of the general population exposed to cannabis develop psychotic illness.
Q.Briefly explain the pharmacokinetics of the psychoactive agent ∆9-tetrahydrocannabinol (∆9-THC).?
Looking at the pharmacokinetics of the psychoactive agent ∆9-tetrahydrocannabinol (∆9-THC), its effects are perceptible within minutes. ∆9-THC is extremely lipid soluble and can accumulate in fatty tissues reaching peak concentrations in 4 to 5 days. It is then slowly released back into the body, including the brain, reaching high concentrations in the neocortical, limbic, sensory, and motor areas.2 The tissue elimination half-life of ∆9-THC is about seven days, and absolute elimination of a single dose may take up to 30 days.
When he was admitted the second time, his behavior was more exaggerated than the first hospitalization. Being that his drug test came back positive for cannabis, we felt strongly that this was another case of cannabis-induced psychosis. Based on pharmacokinetics, a single dose of ∆9-THC may last for an absolute period of 30 days. However, when his symptoms had not abated after one month with no treatment, we changed our working diagnosis to bipolar disorder with psychosis being that he showed both affective and psychotic symptoms.
Since his symptoms resolved with these medications, we feel that the cannabis affected his neurochemical system in a chronic way causing him to have long-term problems. As our case report demonstrates, there are individuals who are otherwise healthy, with no genetic predisposition, who can be diagnosed with a psychiatric illness purely with cannabis abuse. This goes along with the first hypothesis that cannabis use causes psychotic symptoms in an otherwise healthy individual, which would not have occurred with abstinence.
“DRUGS TAKE YOU TO HELL, DISGUISED AS HEAVEN.” – Donald Lynn Frost.