Bipolar Depression
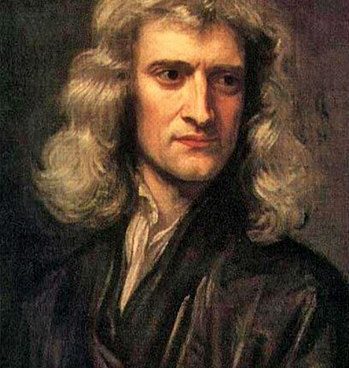
“I Can Calculate The Motions Of Heavenly Bodies, But Not The Madness Of People” – Sir Isaac Newton.
Case study # 3.
29-year old Jane presented with a history of recurrent and disabling depression and headaches. Several weeks prior to presentation, she became severely depressed and had difficulty moving, had diminished appetite, had crying spells much of the day and felt suicidal.
The surest sign of a phase of depression is that you feel down for a long time — usually at least 2 weeks. You might have these episodes rarely or several times a year.
What Is The Difference Between Unipolar Depression & Bipolar Depression?
Unipolar depression would be depression symptoms without mania.
Symptoms of unipolar depression still match the “downside” of bipolar.
Doctors looking to diagnose unipolar depression will look for criteria that might support such a diagnosis. For example, anyone who does not experience manic episodes, or who recently suffered a death in the family or some other life-altering issue, would probably be suffering from unipolar depression. Tragic events cause sadness and the negative feelings can linger. Drugs and physical disease can cause depression, even severe depression, without there being symptoms of unipolar or bipolar depression. In fact, according to B.A.D.S., doctors now believe that major depressive disorder cannot be due to bipolar disorder. They are different conditions caused by different factors.
At the time she presented, she was on Prozac 20 mg a day, and described herself as getting “manicky” on the Prozac. By this, she meant that she was “rushing around, laughing a lot and having more anxiety.” A past trial with Wellbutrin was poorly tolerated because of sweating episodes, insomnia and agitation. Her depression was worsening despite the Prozac treatment.
DSM-5 now considers that mood elevation with antidepressants justifies the diagnosis of bipolar disorder, whereas earlier editions considered it a drug-induced reaction.
In November 2013, Psychiatric Times published an article by Ross Baldessarini, MD, a Harvard psychiatrist, et al titled ‘Switching’ of Mood From Depression to Mania With Antidepressants. click here to read more,
In DSM-IV, incidents of this kind were excluded:
“Note: Manic-like episodes that are clearly caused by somatic antidepressant treatment (e.g., medication, electroconvulsive therapy, light therapy) should not count toward a diagnosis of Bipolar I Disorder.” (p 332) [Emphasis added]
But in DSM-5, this has been changed to:
“Note: A full manic episode that emerges during antidepressant treatment (e.g., medication, electroconvulsive therapy) but persists at a fully syndromal level beyond the physiological effect of that treatment is sufficient evidence for a manic episode and therefore, a bipolar I diagnosis. (p. 124) [Emphasis added]
The diagnosis of major depressive disorder was suspect, given the poor response to both antidepressants. Prozac was discontinued because it appeared to be worsening the underlying mood swings.
Family history revealed severe mood swings in both her father and paternal grandmother. Grandmother at times would take to bed for long spells, and she had been hospitalized for “unknown reasons” that the family refused to talk about, and the client recalled that the secrecy was because of something “shameful” about her grandmother’s condition and behavior.
She also described a history of mood swings for many years.
A medical professional might look beyond peripheral symptoms to determine more detail-oriented observations like:
- Appearance of mania in childhood
- Number of depressive or mania episodes
- Non-response to anti-depressant medication
- Rapid response to anti-depressants
- Family history of bipolar
- Relationship history, especially erratic or impulsive behavior
- Job history, especially erratic or impulsive behavior
- Legal issues and criminal record
- A history of drug abuse
Because of the suggestion of Manic Depressive / Bipolar Disorder by personal and family history, she was placed on Quetiapine 100 mg at bedtime. Within one week’s time, she began to improve markedly, including clearer thinking, more productive work being done, less depression and more energy. Within five weeks after the institution of Quetiapine, the client was feeling “terrific.”
Bipolar disorder II is somewhat difficult to diagnose, in comparison to Bipolar I, since hypomania can be missed, or exaggerated in the mind of the patient or even the doctor to be mania. One point the doctor will make is to determine what the “primary mood” is-and in Bipolar it is usually irritability, and not the “high” euphoria spells.
Bipolar I phases are usually “very pronounced” and hard to miss since mania episodes are extreme. The hypomania involved Bipolar II can be mild with major depression.
Bipolar II disorder: This diagnosis is given when a patient has had at least one depressive episode and a period of elevated mood referred to as hypomania. Bouts of hypomania are not as extreme as mania and are shorter lived. Patients with Bipolar II tend to experience longer depressive episodes and shorter states of hypomania. Patients often seek treatment during the depressive episode, as the hypomanic symptoms might not impact functioning as much.
“THE BRAVEST THING I EVER DID WAS CONTINUING MY LIFE WHEN I WANTED TO DIE” – Julliette Lewis.